With support from the US Army Medical Research and Development Command’s Combat Casualty Care Research Program and MTEC, the Alam Trauma Basic and Translational Science Laboratory at Northwestern University has shown that the use of a new partial resuscitative endovascular balloon occlusion of the aorta (pREBOA) can drastically increase the time of aorta occlusion from 30 minutes to over 4 hours with manageable side effects.
Hemorrhage remains the leading cause of death from trauma. The introduction of tourniquets for compressible extremity hemorrhage and other tactical combat casualty care interventions have improved outcomes for battlefield injuries. However, non-compressible torso hemorrhage (NCTH) remains a leading cause of preventable death in both the civilian and military settings. NCTH is seen in 32.7% of potentially survivable lethal combat injuries. Control of NCTH requires interventions that are not typically available in the pre-hospital setting; therefore, the associate mortality rates remain extremely high.
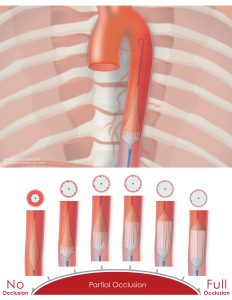
In this project the Alam Lab evaluated the practical feasibility, strategies for use, and appropriate injury patterns for the clinical utility of the pREBOA-PRO (Prytime Medical). The resuscitative endovascular balloon occlusion of the aorta (REBOA) is a strategy for providing temporary control of ongoing hemorrhage in traumatically injured trauma patients by occluding the aorta. While the device has been used in both military and civilian settings over the past couple of decades, there are notable limitations. Complete aortic occlusion results in distal ischemia severely limiting the recommended inflation time to 30 minutes. In turn, this limits the clinical utility of the device. The pREBOA-PRO is a partially occluding REBOA that addresses those limitations by allowing blood to flow beyond the balloon to perfuse the organs. This study is the first to use the third generation pREBOA-PRO to show that the zone 1 aorta can be occluded for over 4 hours with histologically survivable and surgically manageable downstream injuries in a swine model. Increasing the potential occlusion time would have major implications in expanding the clinical utility including aeromedical transport, long distance transfers, or austere field placement.
For the next steps in the project, the Alam Lab will evaluate the efficacy of using the pREBOA-PRO to obtain proximal hemorrhage control and stop bleeding from an uncontrolled hemorrhage. Additionally, they will evaluate the use of the pREBOA in traumatic brain injury. Translational science laboratories allow for standardized testing of novel devices to optimize clinical use in humans. They have developed a consistent model that allows for further testing of the pREBOA-PRO and look forward to continuing to clarify the technical use, patient population, and indications of the device in the coming years.
This work has been recently published in the Journal of Trauma and Acute Care Surgery. The research project award recipients were selected from the respondents to MTEC’s Request for Project Proposals soliciting medical technological solutions related to MTEC’s Technology Focus Areas (Solicitation #MTEC-17-08-MULTI-TOPIC).
About Northwestern:
The Alam Trauma Basic and Translational Science Laboratory is focused on developing and testing novel interventions for improving care of trauma patients. Our long-term goal is to improve the outcomes of trauma victims by identifying and validating new and effective treatment strategies for rapidly lethal insults such as hemorrhage, traumatic brain injury, severe sepsis and poly-trauma. We are especially interested in treatments that can be delivered in austere settings, such as a battlefield and pre-hospital environment.
The research team is led by Dr. Hasan Alam, a trauma surgeon at Northwestern University, Feinberg School of Medicine. In addition to being a practicing trauma surgeon, he is a translational scientist, and clinical investigator, with expertise and research interest in the areas of sepsis, hemorrhage, resuscitation, bleeding control, novel cell protective strategies, and traumatic brain injury. He is also the Loyal and Edith Davis Endowed Professor and Chair, Department of Surgery and Professor of Cell & Developmental Biology at Northwestern University Feinberg School of Medicine; and Surgeon-in-Chief, Northwestern Memorial Hospital In short, he brings more than 2 decades of experience with funded research, mentoring, and academic leadership to this project. The laboratory is staffed with a post-doctoral fellow and general surgery resident, Dr. Jessie Ho, who serves as the main project leader for this work. Additionally, this work cannot be completed without the technical support of our large animal veterinarian, Kiril Chtraklin, and a culture of collaboration and collegiality with the Northwestern Center for Comparative Medicine. The technicians and staff on the team are invaluable in supporting the work required to conduct experiments.
Copyright 2023, Prytime Medical Devices, Inc. All rights reserved. Reprinted with permission.
Disclaimer: The views expressed in this news article are those of the authors and may not reflect the official policy or position of the Department of the Army, Department of Defense, or the U.S. Government.





